Now is the Time for the Adaptive Hospital
November 2020


Pandemic-proofing with modular adaptations and smart technology
One thing is clear—Covid-19 has had a major impact on our lives, society and health care. And although we certainly don’t believe that the pandemic will continue to dominate our lives forever, we can’t deny that Covid-19 has been a rough wake-up call. Hospitals need to be more flexible and stress-resistant. The architects at Wiegerinck and engineers at Deerns have come together to sketch out a vision for the adaptive hospital. Together, we have created a relatively simple and financially viable plan to make your hospital “pandemic proof”.
Simply put, an adaptive hospital is one that is set up in such a way that it can accommodate infected patients without disrupting regular care. The goal is to have a designated zone within the hospital that can be quickly and easily converted for crisis care in an emergency situation (e.g. a virus outbreak or chemical contamination). Viruses pose a major threat to vulnerable patients and staff, and since the current coronavirus measures have proven insufficient, we need to focus more intensively on physical and structural adaptations. So, what does an adaptive, pandemic-proof hospital look like?
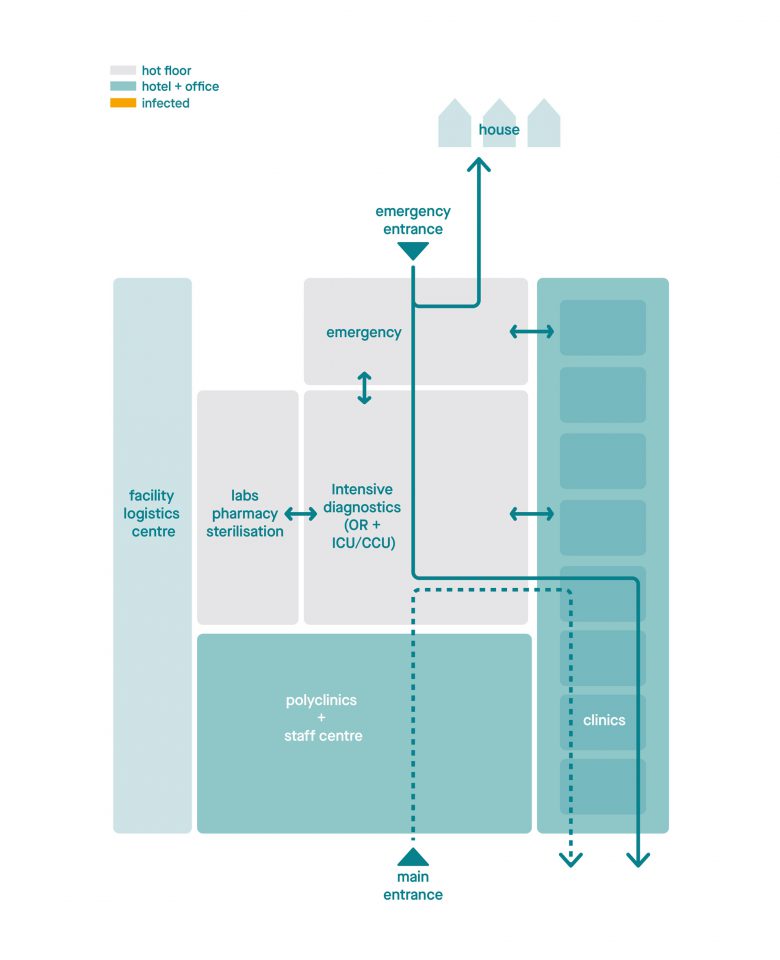
The 'normal setting'. The hospital has a clear separation between the hot floor and (poly)clinics and office. Functions are positioned in such a way that the walking routes/flows are clear.
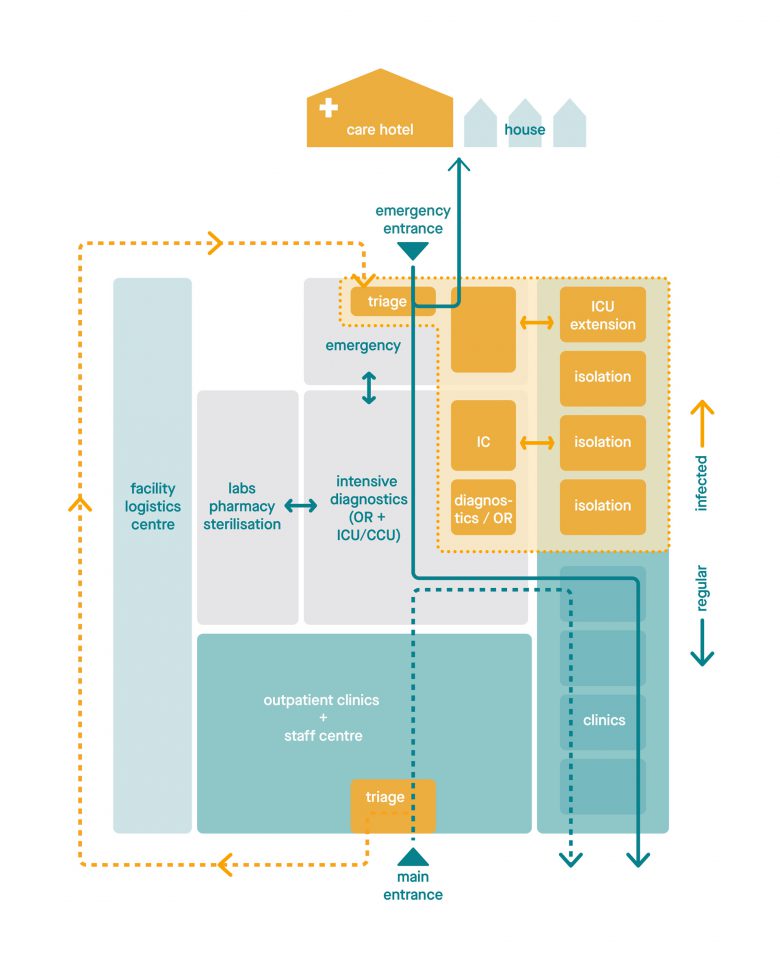
The 'crisis setting'. Part of the hospital is quickly converted, with a closed circuit for infected patients and an emergency hospital. Regular care can continue undisturbed.
The ideal
Naturally, our ultimate goal is to design and build the perfect hospital; hence, the solutions discussed in this article are largely based on our vision for the ideal adaptive hospital. That said, with a few relatively simple interventions at a manageable cost, your hospital can be made more adaptable and future-proof too. The adaptive hospital consists of the following steps:
- Creating an emergency hospital within the hospital
- Implementing a modular design
- Integrating smart building technology
- Making more use of e-health solutions
One hospital, two settings
In our scenario, an adaptive hospital has two ‘settings’: a ‘normal setting’ and a ‘crisis setting’. In the ‘normal setting’, hospital care runs smoothly, just the way we like it. In the ‘crisis setting’, however, acute specialist care can be provided to a specific group of patients, with as little negative impact on regular care as possible (staff capacity permitting, of course).
Modular design
The basic idea behind modular hospital design is to determine in advance which parts of the building can be immediately adapted and compartmentalised in the event of an emergency in order to provide acute, safe crisis care. Ideally, the rest of the hospital (though slightly smaller) should be able to continue normal operations undisturbed. This modular architectural and installation-technical design ensures that crisis care and regular care can take place side by side. In essence, we are creating an independent, pop-up emergency hospital within the larger hospital.
A hospital within a hospital
The emergency hospital within the larger hospital can be up and running almost immediately in the event of a large-scale outbreak, like Covid-19. The emergency hospital has a separate entrance with triage, and from there it forms a closed circuit with an emergency department, clinical patient rooms and an ICU. If necessary, a diagnostic room and OR can be safely implemented as well. From the separate triage entrance, the patient can either be sent home, checked into a care hotel or enter the hospital. If hospitalisation is necessary, the patient enters via a segregated section of the emergency department. From there, a safe route leads to the ICU or a pre-allocated nursing ward.
Quick addition and removal of IC beds
Within both the ICU and the special emergency department, extra sealable doors have been installed so that the number of beds in a safe compartment can be increased or reduced as needed. Some rooms are large enough to accommodate a second IC bed, offering extra flexibility. Another option is to make the rooms within the emergency clinic ‘acuity adaptable’, so that—from an installation point of view—they are fully suitable for crisis care. Examples of such innovations include creating facilities that are able to connect to mobile IC units, upgrading local ventilation systems, and limiting the expansion of both the air transport system and the central air pre-treatment system.
Clustering clinics
Less critical patients are taken via a safe circuit and separate lift to a sealed, clinical ward within the emergency hospital. Here, too, the wards should have a modular design. By subdividing the clinical department into modules, it becomes possible to scale up the emergency hospital step by step, per cluster.
In the scenarios we’ve used, most of the structural and technical measures have been integrated into the design. Only the first clinical clusters are slightly over-dimensioned. They have larger rooms, more technical connections and their own ‘contaminated waste’ circuit. The fire-resistant doors also serve as crisis seals. In short, we’ve designed the building in such a way that only the emergency area needs to be adapted, not the entire hospital. As a result, additional investments and interventions are kept to a minimum. It is a matter of designing differently and creating an alternative access system.

Impression of a family room within the emergency hospital that offers dignified, safe contact. The patient and the partners/family members in the adjoining room can see and hear each other.
Human contact
The ideal hospital also takes family care into account, so that we can avoid the devastating separations of the first corona wave. The emergency hospital needs to afford space for dignified but safe contact between the patient, partners and family members. For example, there is a separate room that allows for visual contact between the (mobile) patient and his or her immediate family members. In the ICU, one way to enable physical closeness is to create a space on the outside of the facade, a kind of gallery where people can have contact with the infected patient by means of audio support. In normal, non-crisis circumstances, this outside space can be used for logistics. This solution has been successfully applied in the Skåne university hospital in Malmö, Sweden, which was specially designed for infectious diseases.
Relieving the burden on staff
In recent months, the pandemic has posed a tremendous challenge to healthcare workers, leading to long hours and more absences. This gives us an urgent reason to consider proven design solutions. Evidence-based design can relieve the burden on healthcare personnel by providing a more pleasant environment where they can work more efficiently and effectively. Decentralised nursing stations and supply storage are two proven solutions that are still not widely implemented in Dutch hospitals. Better logistical design and facility support can certainly relieve pressure on healthcare personnel. Our hard-working health care professionals deserve our utmost attention. The least we can do is make sure they have a pleasant (outdoor) space to relax and unwind. This is just one of the ways that we can show these people we are so proud of that we really care.
And of course, further digitalisation can reduce the burden on staff as well. E-health solutions can help to further optimise staff deployment.
Adapting installation technology
In terms of installation technology, having multiple options can contribute greatly to the adaptive character of any hospital. Here are a few examples of what’s possible:
- The integral application of ‘smart building’ technology can significantly reduce the risks of virus outbreaks. Smart building means that visitor flows, logistics and work processes are optimised and adjusted on the basis of real-time collected data. A ‘smart’ hospital can use this data to prevent errors and monitor and improve staffing, energy consumption and safety.
- Smart building technology improves the ‘patient’s journey’ from home to their specific hospital department. Patients receive real-time information about travel time and the correct route to take in the hospital before they have even left home.
- Dynamic route indication separates infected and non-infected visitor flows.
- A separate tube-mail system from the emergency hospital relieves pressure on the logistic device and reduces the risk of incidents with contaminated material.
- From an infection-prevention point of view, we recommend an ‘all air’ treatment system (with 100% outside air) or a generously dimensioned ventilation system, preferably in combination with a climate ceiling.
- All technical facilities are generously dimensioned, both centrally and at the departmental level, to meet possible future requirements.
- In the event of a calamity, the ventilation system of the cohort department can be switched in such a way that the exhaust air is sent directly outside.
- For severely weakened patients, additional protective devices may be considered, such as separate wastewater discharge and the application of backflow protection and thermal disinfection.
What about your hospital?
Your hospital has undoubtedly been faced with these important questions too. What should we do? How can we make the hospital pandemic-proof? What investments are feasible and justifiable?
The speed at which Covid-19 has ‘taken over’ our healthcare system shows just how important it is to take a critical look at the current situation. No one in healthcare ever wants to be surprised by a major virus outbreak again. In principle, many aspects of our ideal adaptive hospital design can be implemented in your hospital as well, though, of course, the specific approach will differ per building.
Emergency hospital study
Together with experts from your team, we can research the ideal size and location for your emergency hospital. This is a study in which the second entrance—the emergency department—will be considered in relation to the placement of additional IC (beds) and the separate nursing ward within the hospital. Thus, it is important that we first create an optimal provisional layout and floor plan with the emergency hospital already integrated into it. Some of the functions within the hospital may have to be relocated in order to ensure that the ‘contaminated flows’ can move autonomously. Safe routing is absolutely crucial.
Determine technical modifications
Based on the new provisional layout, we can then consider the desired structural and technical modifications together. Here are a few examples of what we can do:
- We can isolate and compartmentalise the emergency hospital in such a way that harmful effects can be even more effectively contained in the event of an emergency.
- We can create acuity adaptable rooms to increase IC capacity. Normally, these beds are part of the regular care process, but they can also be upgraded in the event of a pandemic. Solutions include mobile units with integrated med-tech equipment, connection points, a vacuum pump, UPS and patient safety supplies, such as an MES transformer.
- We can install a sluice (temporary and inflatable, if necessary) on the boundary between the emergency hospital and the rest of the hospital, where staff can put on and remove protective equipment. If possible, this area should be pressurized to prevent the spread of unwanted particles.
- We can apply plug-and-play ventilation systems to existing openings in the façade. This ensures that individual rooms are disconnected from the central installations and have an independently functioning climate system that can also maintain a pressure hierarchy.
- We can make sure that the existing ventilation system mirrors the current guidelines (the current vision is that the guidelines are sufficient to control Covid-19). Once we have checked that everything is working properly, we will optimise the system where possible and draw up an operational plan for management and maintenance. Ideally, the emergency hospital should be pressurized in relation to the rest of the hospital.
- We can offer a form of triage at the main entrance to the regular care hospital.
- We can create spaces for visiting family members.
- We can increase the amount of (outdoor) space, where staff can recover from the heavy toll of the pandemic.
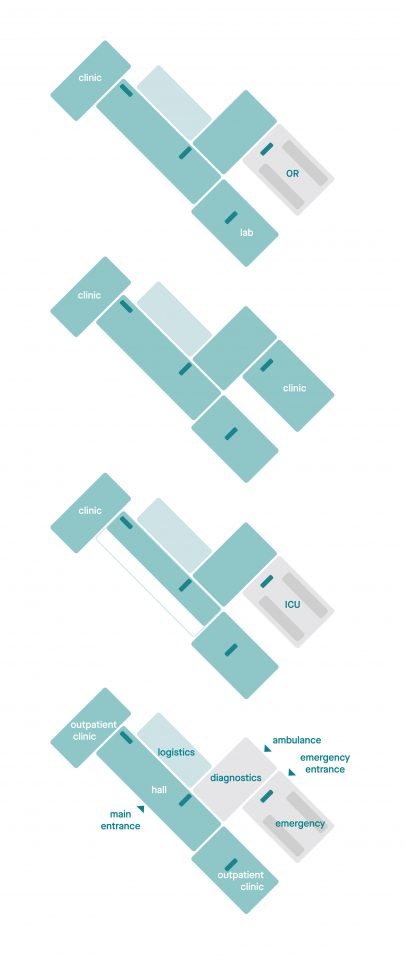
Schematic representation of the care facilities within a hospital. Polyclinics close to the entrance, patient tower and a stacked hot floor with an emergency entrance.
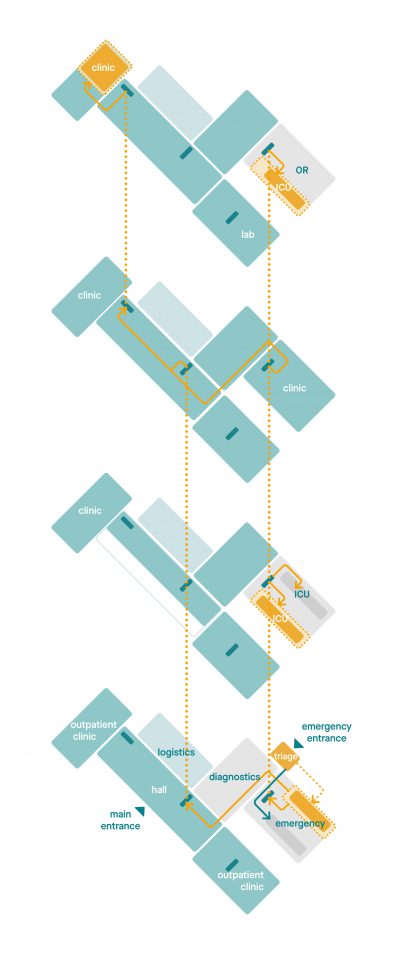
During the first corona wave, ad hoc adjustments were needed to provide acute care. This led to situations where infected patients were spread throughout the hospital, severely hampering regular care.
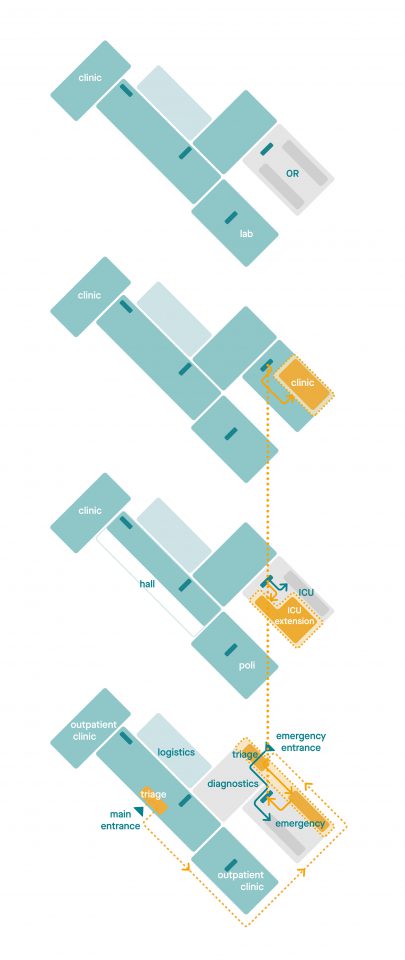
By exchanging a limited number of functions, a compact emergency hospital can be created within any existing hospital. As a result, regular care can continue unhindered even in crisis situations.
Now’s the time to plan ahead
Covid-19 has shown us that it’s time for a change. Hospitals need to become more stress-resistant so that, in the event of another pandemic, they can quickly adapt without having to resort to ad hoc solutions. By anticipating future viral outbreaks, hospitals are automatically investing in an effective solution for other diseases and calamities. In short, now is the time to start thinking about the optimal layout, routing, compartmentalisation and ventilation systems for your hospital, as well as how you can further integrate e-health and smart building technologies. With relatively limited interventions at a manageable cost, your hospital can become adaptive too!
This article is a follow-up to our previous publications, ‘Hospitals after Corona’ by Wiegerinck and ‘Aerogenic spread of SARS-CoV-2′ by Deerns. In this joint sequel, we present our vision for the adaptive hospital and indicate what such a hospital might look like. Based on this vision, we can advise hospitals on how they can use our insights to create an integrated architectural and installation plan.


