Post-Corona Hospitals
July 2020


Working together towards
a “pandemic-proof” hospital
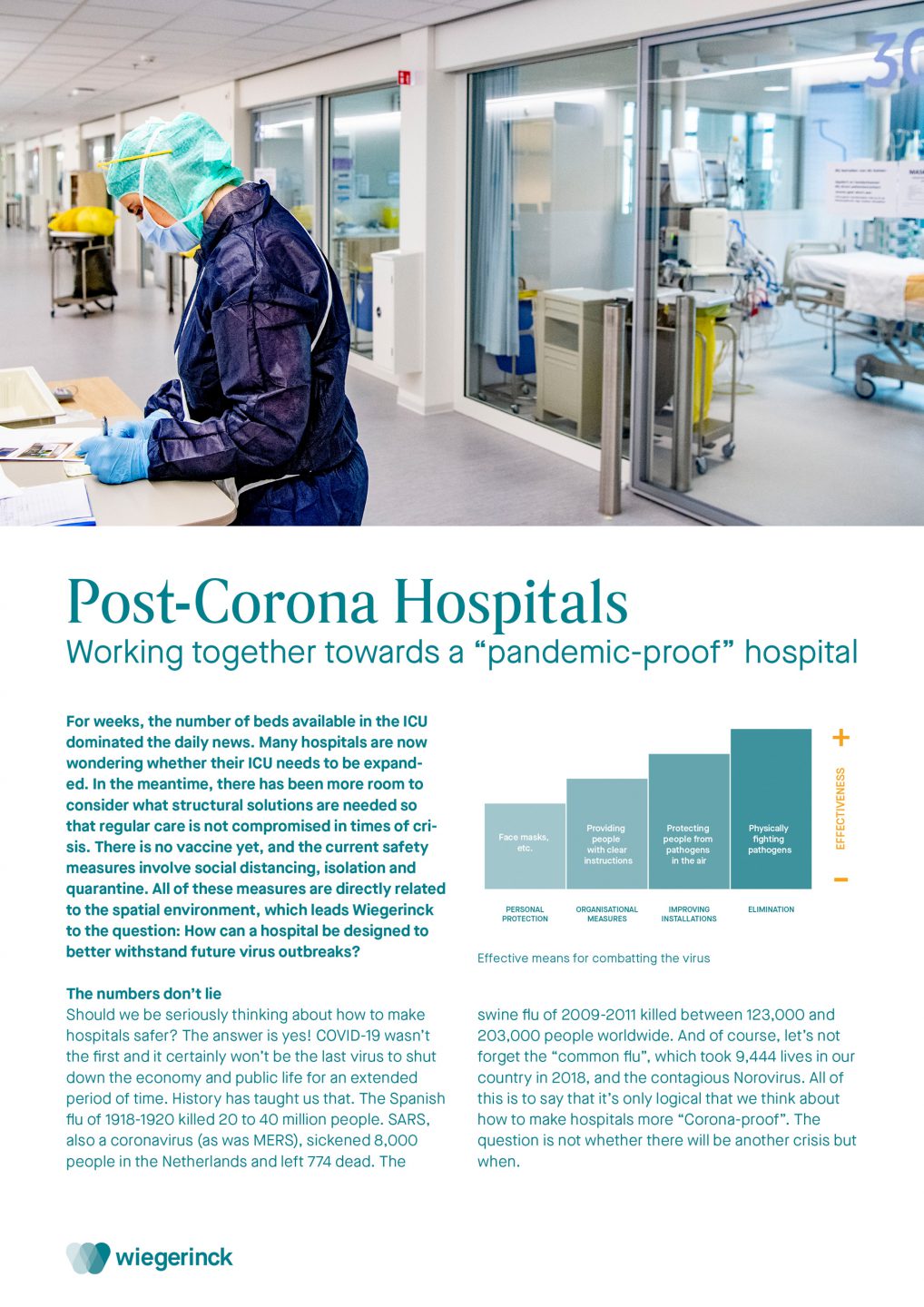
For weeks, the number of beds available in the ICU dominated the daily news. Many hospitals are now wondering whether their ICU needs to be expanded. In the meantime, there has been more room to consider what structural solutions are needed so that regular care is not compromised in times of crisis. There is no vaccine yet, and the current safety measures involve social distancing, isolation and quarantine. All of these measures are directly related to the spatial environment, which leads Wiegerinck to the question: How can a hospital be designed to better withstand future virus outbreaks?
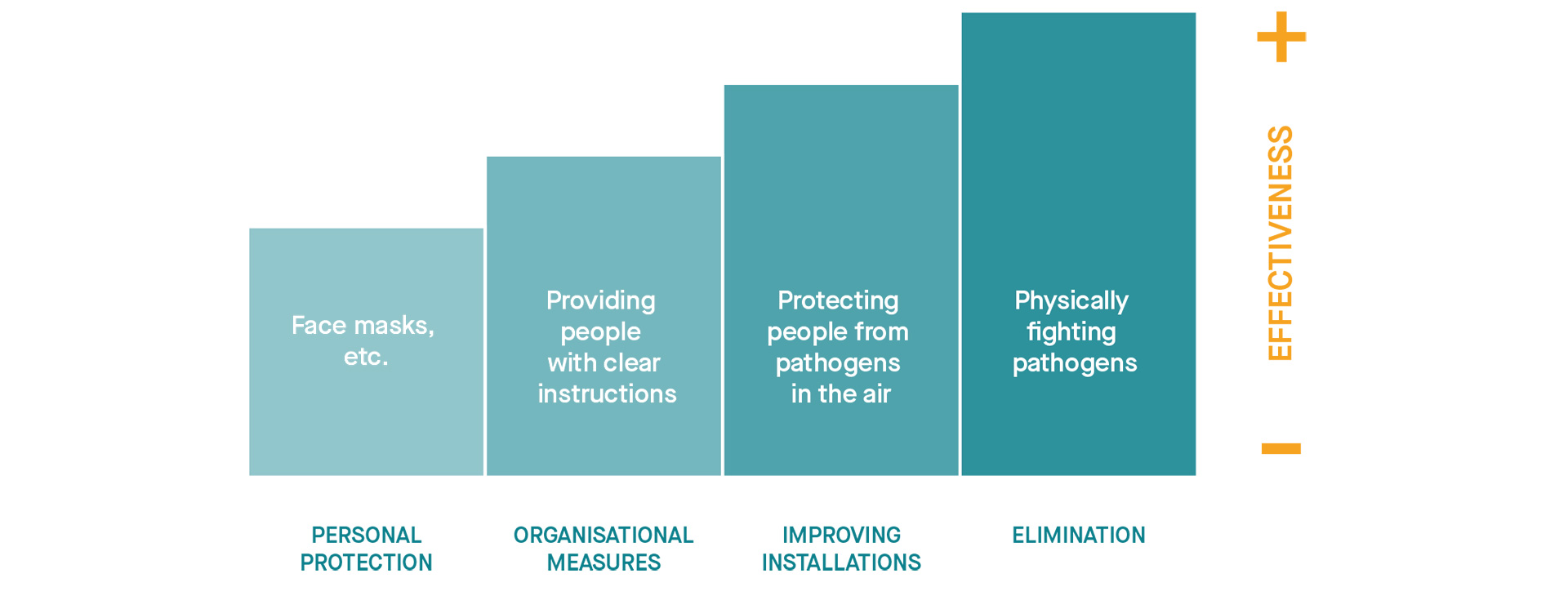
Effective means for combatting the virus
The numbers don’t lie
Should we be seriously thinking about how to make hospitals safer? The answer is yes! COVID-19 wasn’t the first and it certainly won’t be the last virus to shut down the economy and public life for an extended period of time. History has taught us that. The Spanish flu of 1918-1920 killed 20 to 40 million people. SARS, also a coronavirus (as was MERS), sickened 8,000 people in the Netherlands and left 774 dead. The swine flu of 2009-2011 killed between 123,000 and 203,000 people worldwide. And of course, let’s not forget the “common flu”, which took 9,444 lives in our country in 2018, and the contagious Norovirus. All of this is to say that it’s only logical that we think about how to make hospitals more “Corona-proof”. The question is not whether there will be another crisis but when.
Architecture and health
Florence Nightingale demonstrated as early as the nineteenth century that the physical environment had even more effect on wounded soldiers than the healing of their initial injury. Wiegerinck is always interested in how architecture can contribute to health, and we’re constantly gaining knowledge thanks to Evidence-Based Design (EBD) research. We stay abreast of the latest publications and research on diseases like SARS, for example, and the lessons we can learn for the future.
How can we prevent a virus outbreak from endangering the primary care process by adapting the physical hospital environment? And what are the critical points in that process in the event of an epidemic?
Critical steps: triage and the ER
Which incoming patients are infected with the virus and which aren’t? During the Corona crisis, this has been a critical point in the care process. For safe patient flow to triage, we are considering ways to cover and/or separate the entrance to the emergency room. Another solution that can be realised relatively quickly is to convert an ambulance hall or parking garage. Other design solutions, such as drive-through or pop-up triage outside the hospital—which reduces pressure on the emergency room, helps spread patients out and limits the danger to the primary hospital—are already being applied. We also expect e-health triage to play a greater role in the future. This could require new kinds of consulting rooms that are more suitable for video calling. Thanks to digital technology and video, many patients have already been diagnosed before they arrive at the hospital and can immediately head to the right department.
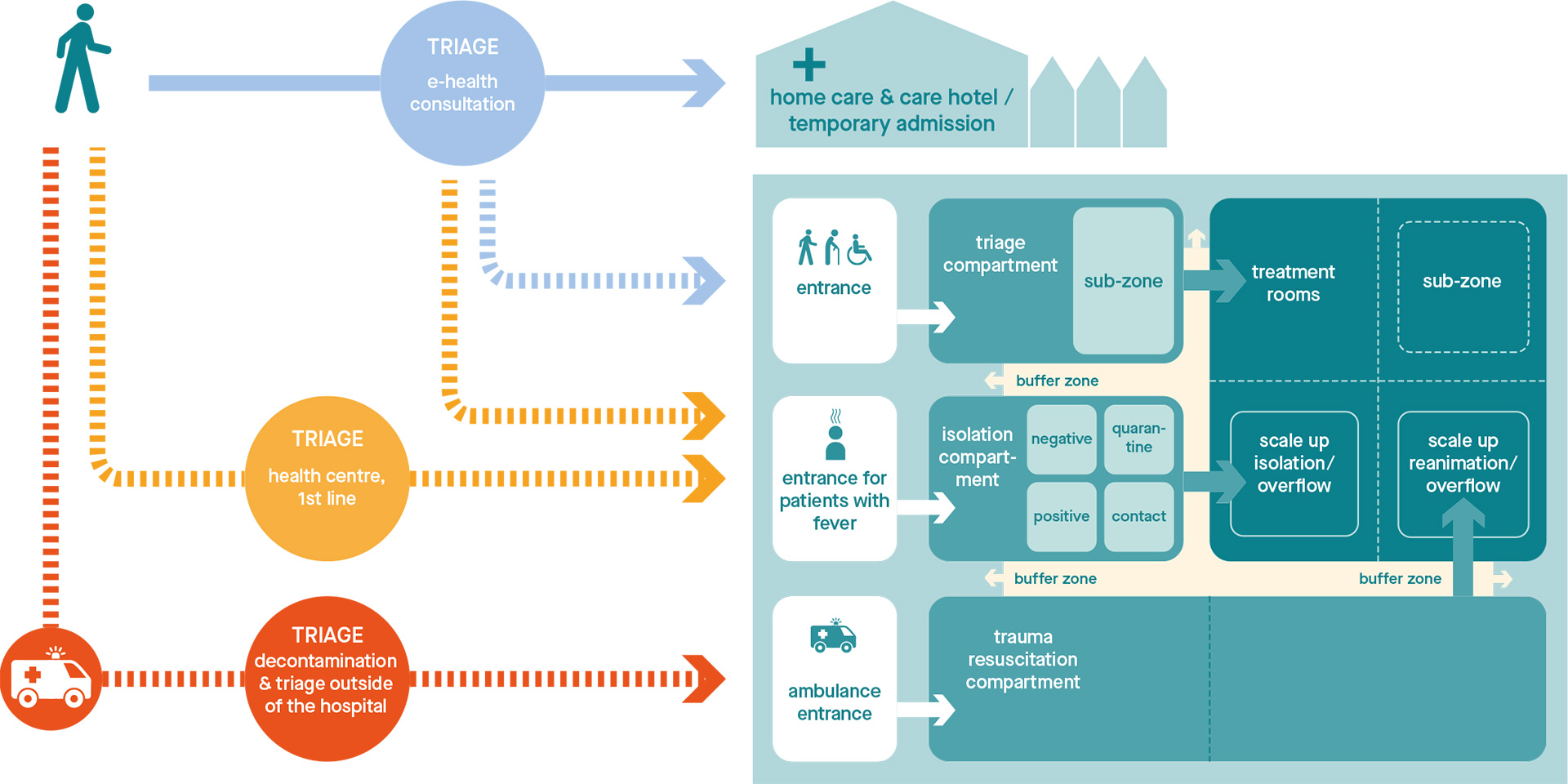
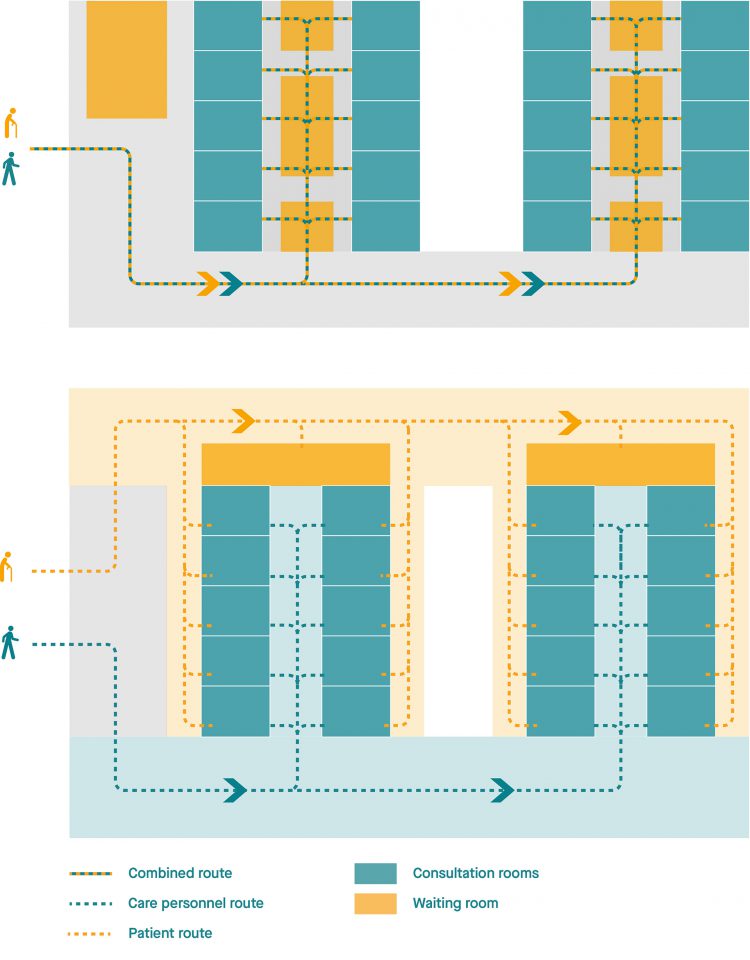
Various separation options
Separating flows
It is important to look at how patients are transferred to the ICU, (isolation) rooms or other segregated wards after triage. Inevitably, we will have to pay more attention to routing, compartmentalisation, and buffer zones—both in new construction and the renovation of existing hospitals. Currently, many hospitals are also considering whether measures such as one-way routes are necessary. Separating patient flows and staff routes (for doctors, nurses, cleaning personnel, food, logistics, etc.) is becoming an increasingly integral part of any design, and keeping people separate is already recommended by EBD.
Effective separation of front and back office
This sample design sketches a structure with a central corridor for patients/visitors. A series of consultation and examination rooms separate the back-office area for medical professionals from the central corridor. Separating patient and staff flows (or in other words, the front and back office) is an effective preventive solution.
The virus and its effects on health care
In the coming period, we will gain a clearer picture of the consequences that the extreme Covid-19 measures have had on regular care. Studies on SARS, for example, have taught us that, at various hospitals, it took several months to a year and a half for all care processes to return to normal. Ultimately, how will the delay in care caused by Covid-19 damage public health? And is such a delay justifiable? Wouldn’t it be better to move some specialists away from the hospital, so that they can continue to safely provide care under any circumstances? These are all legitimate questions that we would like to find an answer to.
Risk as a starting point
In our opinion, the risk of an epidemic or other crisis situation should be an important starting point when designing a new or renovated hospital. For example, thinking about how the building can be adapted quickly in the event of a virus outbreak. EBD shows that single rooms are the safest solution in terms of patient health. Physical isolation of patients—from admission to discharge—is best, precisely because it is often not known whether someone is carrying a virus or bacteria. EBD has been advocating standardized construction for years, making departments and rooms flexible and easy to scale up when the need arises.
Standardisation, a big step forward
A hospital building, whether new or existing, can be designed or renovated based on clear compartmentalisation strategies. Nursing wards and ICUs, as well as part of the emergency room, can be separated from other care processes in the event of a virus outbreak and serve as a shelter for infected patients. The rest of the hospital can continue to operate in a scaled-down form where necessary. Of course, this is not only a construction issue, it’s also an installation issue. After all, the “compartments” must be designed in such a way that the various building components can function independently.
Outpatient benefits of e-health
The Corona pandemic is likely to give an enormous boost to e-health services in hospitals. Patient flows can be much better regulated thanks to e-health methods. This will have a particularly large effect on specialized outpatient clinics, where the largest people flows are usually found. A significant portion of the intake interviews, registration, check-up and follow-up appointments can be done safely online via a video link. The patient is at home with his/her smartphone, tablet or laptop, and the doctor or nurse is in an e-consultation room with a good camera and proper lighting and acoustics. By using a digital login system and a real-time consultation app, we can considerably reduce the number of people waiting around in the hospital.
More space, healthy routes
Wide entrances that give way to spacious entrance halls, where one can easily keep a distance, are likely to become a reality in all hospitals. Throughout the building, the accumulation of people will have to be avoided as much as possible. Entrances and exits will be chosen in such a way that the flow of people—both healthy and infected—will be easily manageable. The number of waiting rooms will be reduced, while the distance between seating areas will have to be widened. Depending on the situation, we can also consider alternative solutions, such as sending patients directly to their consultation room and having the doctor make rounds to patients. In that case, registration and follow-up appointments will be organised differently. Registration will take place at home and follow-up appointments will be scheduled on the spot, in the consultation room or at private, closed desks.
Changes to the nursing environment
Limit contact and maintain distance. These will also be the new starting points in nursing wards, treatment environments and day treatment facilities. If a patient can be admitted “without bed”, he or she does not have to stay in the nursing ward unnecessarily. Should there be two metres between the beds now that the 1.5-metre distance will probably be increased to six feet? Is a bed curtain really enough to reduce the spread of pathogens?
In the United States, we’re already seeing examples of cubicle-like spaces, and the general trend seems to be moving towards closed single rooms, which, according to EBD, are more desirable. Whatever the case, hospitals are increasingly demanding standardized, secure rooms that allow for flexible expansion even during a “normal” flu period.
Staff safety
Designing for health care is not just designing for patients. The health and safety of staff is equally important, as is creating a pleasant and attractive working environment. Medical personnel working intensive shifts need plenty of comfortable space to recover from their heavy workload. This includes a nice, large break room, an outdoor area and places to sleep. Hospitals will need more areas throughout the building where staff can change clothes and equip themselves with the prescribed personal protective equipment. These spaces shouldn’t be too small, as small spaces increase the risk of viral contamination. Attention for personal protective equipment (face masks, aprons, protective glasses, etc.) was already evident during the SARS outbreaks, and the importance of washing hands upon entering each room and immediately upon returning home has been further emphasized as well. Whether to install (extra) sinks and washing facilities will be a question that every hospital needs to consider.
Effective and efficient cleaning
The quick and effective cleaning of patient rooms and sanitary facilities is essential, especially during an epidemic. But we must also look at the surfaces and materials present in those spaces. SARS could survive six days on a dry surface. And it seems that Covid-19 can survive longer on stainless steel, plastic and composite, whereas on wood, cotton and leather it can only live for 24 hours. The fewer surfaces we touch, the better. We’re already familiar with motion-sensor water taps and alcohol and soap dispensers with elbow levers. Automatic doors, voice control and other hands-free technology can also help us to work “contactless” and help prevent contamination.
During the design process, conversations with hospitals still tend to be overly focused on easy-to-clean floors and walls, but we have to look further. Door handles, lift buttons and stair railings may be even more important when it comes to preventing the spread of infection. For example, one recent study suggests that bacteria cannot survive on copper, making it a potentially good material for door handles. And there are undoubtedly more effective hygienic solutions on the horizon.
Ventilation methods
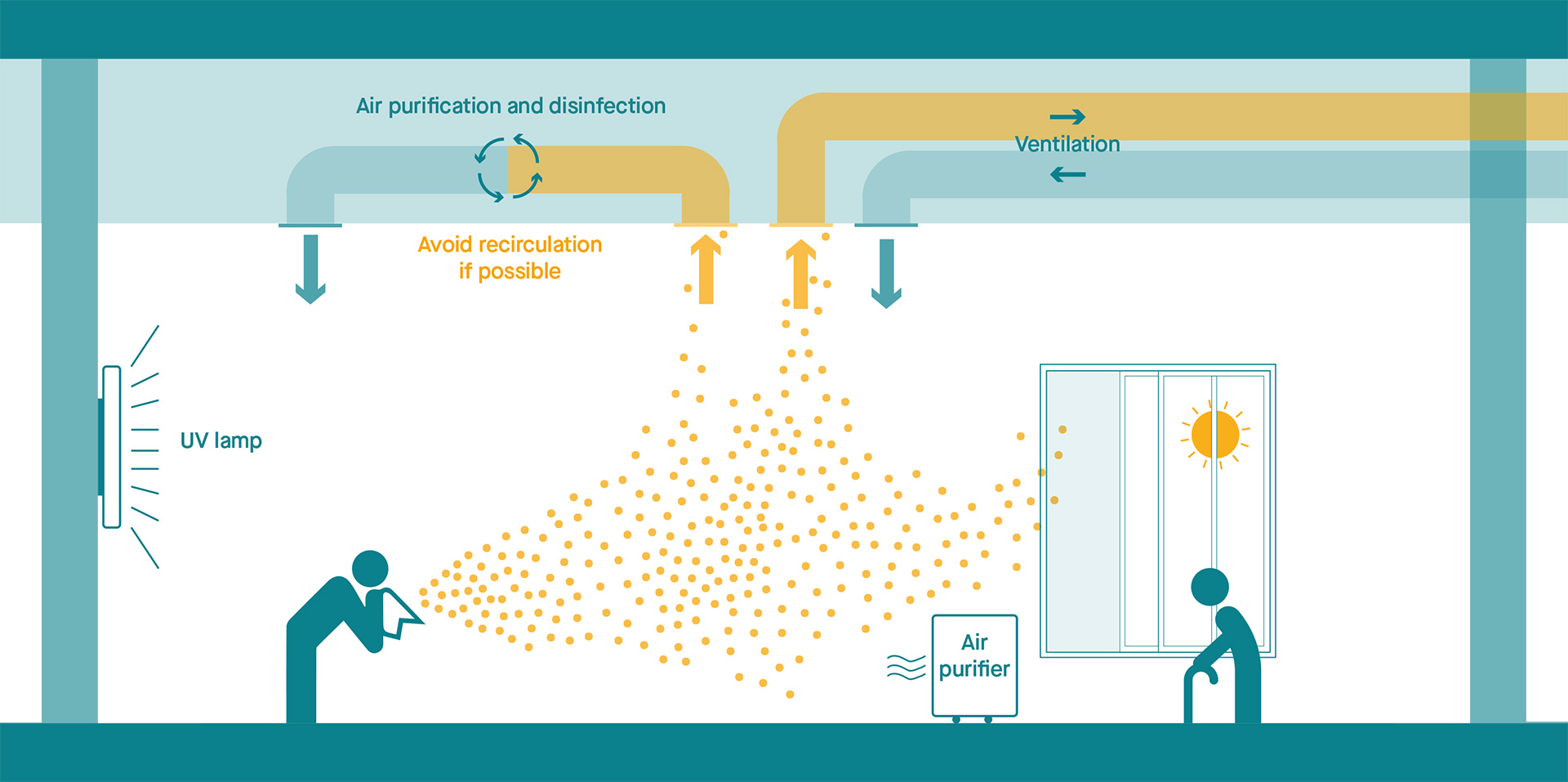
Healthy air
We know that the air circulation in the hospital plays an important role as well. In this respect, Dutch hospitals are already doing quite well. Clean, uncirculated air is the norm and air filtering is generally effective. HEPA filters and GUV/UVGI (ultraviolet) help to filter pathogens out of the air; however, we’ve also learned that HEPA filters had no effect on SARS, whereas a good air pressure regime did. By installing self-closing doors in the right places, we can further improve the air pressure regime. Also, it is highly likely that humidity and temperature influence the spread of viruses like Covid-19 as well. This is certainly the case when it comes to contamination between beds in shared rooms, such as those in the ICU or holding areas. SARS research has shown that high ceilings with ceiling fans and open windows (natural ventilation) result in fewer infections than small rooms without windows.
Compartmentalisation
Separation and compartmentalization are keywords when it comes to the necessary installations. Is it possible to separate a number of ORs during an epidemic so that regular care and treatment can continue safely? Being able to separate is important for any department or room that needs to be able to function independently in the event of an outbreak. Ideas include a stand-alone nursing wing for infected patients or a completely disconnected area in the emergency room. The basic idea is that contaminated air in the building cannot spread beyond the compartmentalised risk zones.
Telemetry
The existing telemetry in hospitals was often a reason for first transforming cardiology departments/stroke units into ICU environments, for example. Thanks to telemetry, the rapid expansion of departments is also possible because intensive care rooms and other rooms are set up for double occupancy. This is yet another argument for standardisation. Standardised nursing rooms on all wards (acuity adaptable rooms) can be adapted quickly and easily as soon as the care demand changes.
Robots in the corridor
Robots could potentially be used to deliver goods and instruments around the hospital and to scan barcodes on items for stock management. This is still largely unexplored territory, but these kinds of solutions are likely to increase in popularity after the pandemic. Keeping medical supplies safe by making sure they’re touched by as few hands as possible could become an important part of improving hospital safety.